Mental health law governs civil commitment procedures, balancing individual rights and public safety for those with mental illnesses or intellectual disabilities. Key aspects include understanding legal frameworks, ethical considerations, and criteria for involuntary treatment. Evaluating mental state, condition severity, and risks is crucial while adhering to strict standards and expert insights. A nuanced approach ensures respect for individual liberties and maintains public safety within the mental health law framework. Reforming civil commitment practices promotes evidence-based community-based treatments and aligns with holistic recovery principles.
In the intricate landscape of mental health law, civil commitment stands as a pivotal concept, shaping the balance between individual freedoms and public safety. This comprehensive guide delves into the multifaceted aspects of civil commitment, exploring its legal foundations, definitional nuances, and ethical complexities. By understanding the fundamentals of mental health law, we can critically assess the rights of individuals while ensuring community protection. Through a nuanced approach, this article navigates strategies for reforming practices, fostering effective treatment, and upholding justice in the realm of civil commitment.
- Understanding Mental Health Law Fundamentals
- Defining Civil Commitment: Legal Frameworks
- Evaluating Individual Rights and Freedom
- Balancing Public Safety and Care
- Ethical Considerations in Commitment Decisions
- Reforming Practices for Effective Treatment
Understanding Mental Health Law Fundamentals
Mental health law is a critical aspect of the legal system that focuses on balancing individual rights and public safety in relation to people with mental illnesses or intellectual disabilities. Understanding this field’s fundamentals is essential for navigating civil commitment procedures effectively. It involves comprehending various legal frameworks, ethical considerations, and specific criteria for involuntary treatment.
Knowledgeable professionals must be adept at interpreting diagnostic assessments, understanding different levels of care, and recognizing when a person meets the legal standards for civil commitment. This process requires a delicate balance, ensuring that the rights of individuals with mental health issues are protected while also providing necessary support and treatment.
Defining Civil Commitment: Legal Frameworks
Civil commitment, a cornerstone within mental health law, refers to the legal process whereby an individual is voluntarily or involuntarily confined in a treatment facility for mental health care. This mechanism is designed to ensure that individuals with severe mental illnesses receive necessary treatment while balancing their freedom and rights against the potential benefits of confinement. The legal frameworks surrounding civil commitment vary across jurisdictions but generally involve specific criteria, such as a diagnosis of a serious mental illness, a substantial risk of harm to self or others, and the need for treatment.
These frameworks typically include provisions for court orders, hearings, and ongoing reviews to assess the individual’s condition and ensure compliance with treatment plans. The goal is to create a structured yet flexible system that respects both the rights of individuals with mental health conditions and the public’s safety. Understanding these legal frameworks is crucial in navigating civil commitment issues, as it enables stakeholders—including lawyers, healthcare professionals, and affected individuals—to make informed decisions within the parameters set by the law.
Evaluating Individual Rights and Freedom

In a comprehensive approach to civil commitment legal issues, evaluating individual rights and freedom is paramount under mental health law. This involves balancing the need to protect society from potential harm with the fundamental rights of individuals, including their liberty and autonomy. Every case requires a meticulous assessment of an individual’s mental state, the nature of their condition, and the likelihood of them posing a risk to themselves or others. Such evaluations must adhere to strict legal standards and evidentiary requirements to ensure fairness and due process.
This process demands a nuanced understanding of various legal frameworks, medical guidelines, and ethical considerations. Mental health professionals play a critical role in these assessments, offering expert opinions on a person’s capacity for decision-making and their potential for recovery. By carefully weighing these factors, legal systems can make informed decisions that respect individual liberties while maintaining public safety, thereby upholding the principles of mental health law.
Balancing Public Safety and Care
In navigating civil commitment legal issues under mental health law, striking a delicate balance between public safety and care is paramount. This involves assessing not only an individual’s risk to themselves or others but also their need for treatment and support. A comprehensive approach must consider the complex interplay of psychiatric conditions, treatment options, and societal norms.
Judges and legal professionals play a crucial role in this process by ensuring that decisions are based on empirical evidence and expert opinions. This includes evaluating the effectiveness of proposed care plans, considering less restrictive alternatives to institutionalization, and constantly assessing whether the individual’s rights and dignity are maintained while addressing public safety concerns.
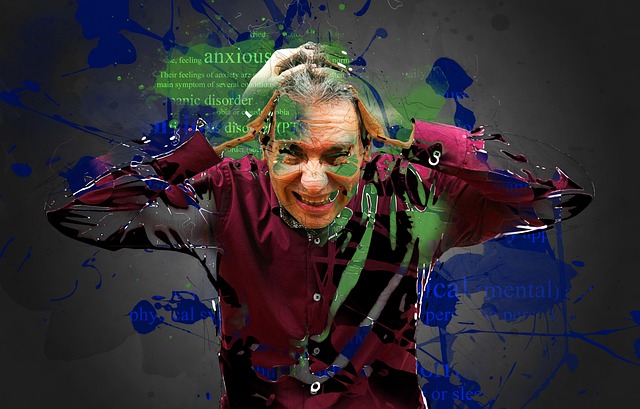
Ethical Considerations in Commitment Decisions
When making decisions regarding civil commitment, a comprehensive approach must incorporate ethical considerations central to mental health law. The primary goal is to balance individual autonomy with public safety, ensuring that the rights and dignity of those facing mental health challenges are respected while preventing potential harm to themselves or others. This delicate equilibrium demands careful evaluation, where factors like informed consent, the risk of injury, and the least restrictive alternative are meticulously assessed.
Ethical dilemmas often arise in cases where symptoms are ambiguous or when an individual’s judgment is impaired. Mental health professionals must navigate these complexities, ensuring their decisions are guided by evidence-based practices and ethical standards. The principles of beneficence, nonmaleficence, and autonomy form the foundation for these considerations, shaping a framework that promotes just and compassionate treatment within the legal framework of mental health law.
Reforming Practices for Effective Treatment

Reforming practices within the civil commitment process is essential to ensure effective treatment and adherence to mental health law. Many systems have historically relied on outdated methods, often leading to prolonged stays in hospitals or institutions with minimal focus on individualized care and recovery-oriented goals. This approach can be counterproductive, as it may perpetuate stigma and fail to address the complex needs of individuals struggling with serious mental illnesses.
To bring about positive change, mental health professionals, legislators, and advocates must collaborate to implement evidence-based practices that prioritize community-based treatment, early intervention, and access to comprehensive support services. This shift would enable a more holistic understanding of an individual’s circumstances, promote their active participation in recovery, and foster reintegration into the community, aligning with principles of mental health law and human rights.